Assignment
I have been given the following cases to analyse and solve, in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and to comprehending clinical data including history, clinical findings, investigations and diagnosis, and then come up with a treatment plan.
This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the medicine assignment based on my comprehension of the cases, divided as per the system concerned:
Pulmonology
Case
1) Evolution of symptomatology 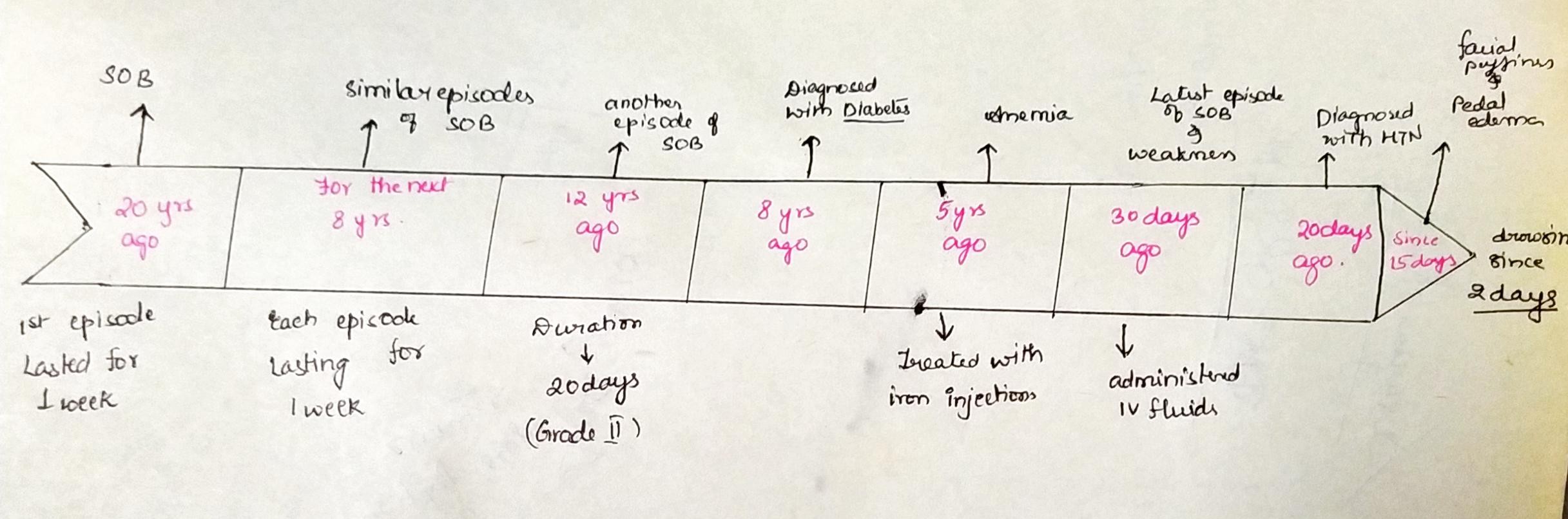
Anatomical localisation:
The cardiovascular sequelae of chronic obstructive pulmonary disease (COPD) have been recognized for decades. The spectrum of cardiovascular disease includes right ventricular (RV) dysfunction, pulmonary hypertension (PH), coronary artery disease (CAD), and arrhythmias.
Vascular remodeling.i.e. Structural changes in the small pulmonary arteries in lungs of patients with COPD involving both intimal and medial thickening in the small pulmonary arteries. However, intimal thickening with components of cellular hypertrophy and hyperplasia have been the most consistently demonstrated morphologic features.
Primary etiology:
In most cases, a COPD exacerbation has direct links to an infection in the lungs or the body.( virus,bacteria or other organisms)
The infection causes inflammation in the lungs. This leads to narrowing of the airways. Blockage occurs due to swelling and mucus production.
Exacerbations might also occur as the result of a severe allergy or inhaling irritating substances from the environment:
organic and non organic dust (hay, paddy field, dander etc)
The following people more likely to have one or more exacerbations the next year:
older adults,
females,
people with reduced lung function,
those who had a history of exacerbations in the previous year,
individuals with a frequent cough that produces phlegm.
(2)Treatment:
Head end elevation :-
A semi-upright position is indicated in ventilated patients. It is recommended to prevent ventilator-associated pneumonia (VAP)
Aspiration of oropharyngeal secretions and gastric contents containing bacteria is considered an essential step in the pathogenesis of VAP.
Head-of-bed elevation (HOBE) is one of several therapeutic interventions that have been demonstrated to reduce respiratory complications associated with mechanical ventilation.
O2 inhalation to maintain SPO2 at 92%
Indications of O2 therapy:
-Hypoxia: (In neonate SpO2 < 88%, PaO2 < 50 mmHg)
-Acute respiratory failure.
-Cardiac failure.
-Shock.
-Severe anaemia.
-Hyper metabolic state.
-During CPR.
-During anaesthesia for surgery and Post operative state
-Seizure.
-Transport of sick patient
-Cyanide poisoning and Carbon monoxide poisoning..
Effects of Oxygen Therapy :
It will decrease the breathlessness of the COPD patients.
Oxygen therapy will help to decrease the weariness in patients.
Oxygen therapy improves the mental condition and mood of the patients.
It will improve one's sleep quality.
Intermittent BiPAP for 2hrs
Indications:
-Chronic obstructive pulmonary disorder (COPD)
-Obstructive sleep apnea
-Obesity hypoventilation syndrome
-Pneumonia
-Asthma flare-up
-Poor breathing after an operation
-Neurological disease that disturbs breathing.
Mechanism:
The machine supplies pressurized air into your airways. It is called “positive pressure ventilation” because the device helps open your lungs with this air pressure.
Inj. AUGUMENTIN 1.2gm IV BO
Indications:
- Acute exacerbation of COPD
-Lower Respiratory Tract Infections.
-Acute Bacterial Otitis Media.
-Sinusitis.
-Skin and Skin Structure Infections.
-Urinary Tract Infections.
-Limitations of Use.
-Serious Hypersensitivity Reactions.
-Cholestatic Jaundice/Hepatic Dysfunction.
Action: Drug binds to PBPS (Penicillin-binding proteins) disrupts cell wall synthesis causing disruption of growth and death of susceptible organisms (bactericidal effect).
TAB. AZITHROMYCIN 500mg OD
Indications:
-Community-acquired Pneumonia.
-Pharyngitis or Tonsillitis.
-Uncomplicated skin/skin structure.
-Acute bacterial exacerbations of chronic obstructive pulmonary disease.
-Acute bacterial sinusitis.
-Genital Ulcer Disease (Chancroid)
-Nongonococcal or Gonococcal Urethritis and Cervicitis.
-Pelvic Inflammatory Disease
Action:
Inhibits protein synthesis by reversibly binding to the 50S ribosomal subunit. Suppression of RNA dependent protein synthesis by inhibition of translocation of mRNA.
Typically bacteriostatic activity
→Bactericidal at high concentrations against very susceptible organisms.
INJ. LASIX IV BO if SBP greater than 110 mmHg
Indications:
Water retention or edema , hypertension.
Action: LASIX inhibits primarily the absorption of sodium and chloride not only in the proximal and distal tubules but also in the loop of Henle. The high degree of efficacy is largely due to the unique site of action. The action on the distal tubule is independent of any inhibitory effect on carbonic anhydrase and aldosterone.
TAB PANTOP 40mg PO OD
Indications:
Gastroesophageal reflux disease, NSAID-related gastric and gastroduodenal injury, Erosive esophagitis, Zollinger-Ellison syndrome, Adjunctive therapy for Helicobacter pylori eradication
Action:
Pantoprazole is a proton pump inhibitor (PPI) that suppresses the final step in gastric acid production by covalently binding to the (H, K)-ATPase enzyme system at the secretory surface of the gastric parietal cell. This effect leads to inhibition of both basal and stimulated gastric acid secretion, irrespective of the stimulus. The binding of pantoprazole to H+K+-ATPase is irreversible in nature, and effectively inhibits acid secretion until a new enzyme is synthesized.
Hydrocortisone
Indications:
-Collagen diseases. Systemic lupus erythematosus.
-Dermatological diseases. Severe erythema multiforme (Stevens-Johnson syndrome)
-Allergic states.
-Gastro-intestinal diseases.
-Respiratory diseases
Action:
Systemic corticosteroids improve airflow,
decrease the rate of treatment failure and risk of relapse,
and may improve symptoms and decrease the length of hospital stay.
Therefore, corticosteroids are recommended by all major guidelines in the treatment of AECOPD.
Existing literature suggests that low-dose oral corticosteroids are as efficacious as high-dose, intravenous corticosteroid regimens, while minimizing adverse effects.
NEB. with IPRAVENT, BUDECORT 6 hrly
Indications:
-Budecort respules are also recommended for use in infants and children with croup (acute viral upper respiratory tract infection ) bronchial asthma(adults), in COPD, in cases in which hospitalisation is indicated.
contain the potent, non-halogenated, corticosteroid, budesonide, indicated for maintenance treatment of asthma and as prophylactic therapy in children.
-Ipratropium bromide is an anticholinergic indicated in the following:for maintenance treatment of bronchospasm associated with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema.
Action:
Ipratropium bromide,
- Relaxes bronchial smooth muscle
may increase mucociliary clearance
act in larger airways
- less effective than sympathomimetics
suitable for prophylactic use
combination is useful.
Pulmoclear
indications: is used to treat and prevent symptoms of chronic obstructive pulmonary disorders such as coughing, wheezing, and shortness of breath. It helps relax the muscles of the air passages thereby making it easier to breathe.
Action: Tablet is a combination of two mucolytic medicines: Acebrophylline and Acetylcysteine. It thins and loosens mucus (phlegm) making it easier to cough out.
chest physiotherapy
Chest physiotherapy techniques such as intermittent positive pressure ventilation and positive expiratory pressure may benefit patients with COPD requiring assistance with sputum clearance, while walking programmes may have wider benefits for patients admitted with an exacerbation of COPD.
GRBS 6 hrly
glucose levels are higher in the airways of people with COPD because inflammation in the lungs makes them leakier so the glucose can move from the blood into the airways.
INJ. HAI SC (8 am- 2pm- 8pm)
Short action insulin to control not glucose levels. Replaces the insulin that is normally produced in the body.
Temp, BP, PR, SPO2 monitoring
I/O charting: Monitoring of Intake help caregivers ensure that the patient has proper intake of fluid and other nutrients. Monitoring of output helps determine whether there is adequate output of urine
INJ. THIAMINE1 amp in 100 ml of NS
treatment of thiamine deficiencies due to increased dietary requirements, reduced intakes, reduced absorption or increased excretion.
(3) causes for Acute exacerbation are caused by a viral or bacterial lung infection, but they may also be triggered by things or situations that make it difficult for you to breathe, such as smoking or being exposed to smoke or air pollution.
(4) Effect of ATT:
yes, ATT could effect her by causing raised RFT, nephrotoxicity. (Rifampin and isoniazid)
(5)Causes for electrolyte imbalance:
Respiratory acidosis with metabolic alkalosis
(due to renal compensation) in AECOPD patients
with chronic hypercapnia is the usual cause of
hypochloremia in these patients.
Common causes of
deranged serum sodium levels include hyperglycemia, use of thiazides or nonsteroidal anti-inflammatory drugs, congestive cardiac failure, chronic renal failure, and low dietary salt intake.
Common causes of hypokalemia include diarrhea, laxative abuse, vomiting, certain diuretics, drugs like insulin, β2agonists, and theophylline.20 Thus, COPD patients per
se are predisposed to electrolyte imbalance. In turn electrolyte imbalance can cause respiratory muscle weakness, cardiac arrhythmia, low cardiac output.
Thus the presence of electrolyte imbalance leads to significantly poor outcome among COPD patients.
References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3700784/
http://rc.rcjournal.com/content/59/10/1583#:~:text=Head%20of%20bed%20elevation%20(HOBE,improve%20oxygenation%20and%20hemodynamic%20performance.
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/bipap
https://copdnewstoday.com/2018/01/09/high-glucose-in-airways-of-copd-patients-may-be-linked-to-increased-bacterial-infections/?cn-reloaded=1
Neurology
CaseA
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
4) What is the reason for giving thiamine in this patient?
5) What is the probable reason for kidney injury in this patient?
6). What is the probable cause for the normocytic anemia?
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
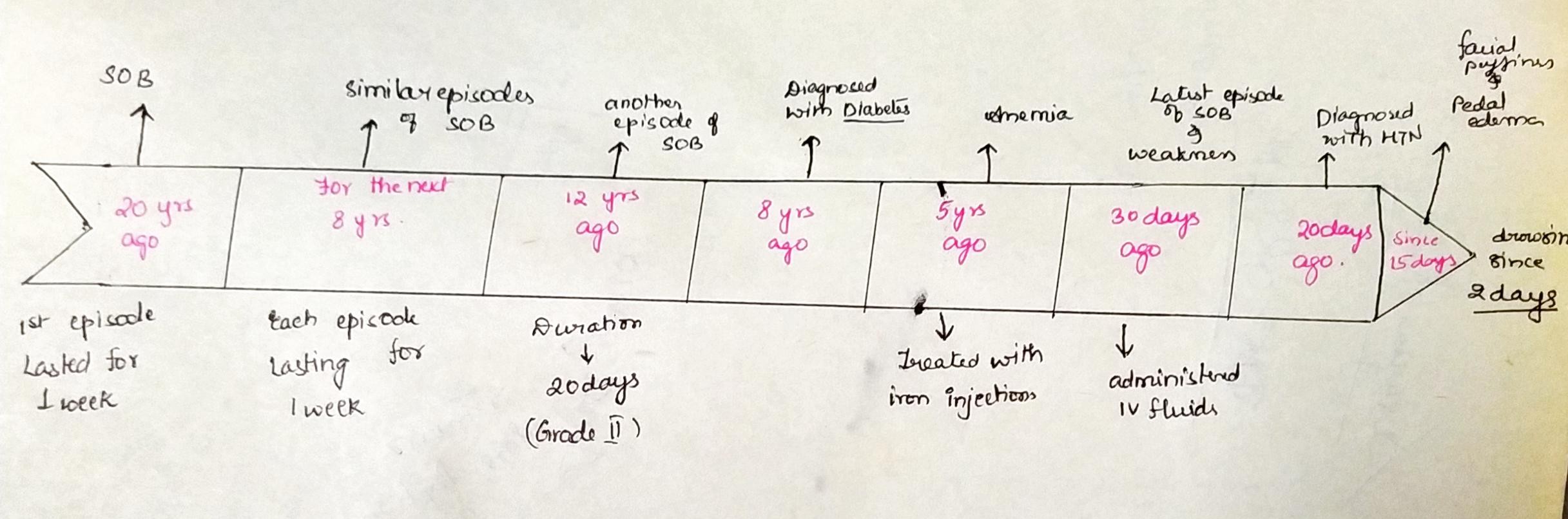
1) Patient has a history of seizures. The timeline of this patient is as follows:
1 year ago- First episode of seizure
4 months ago- Second episode of seizure (24 hours after with the withdrawal of alcohol, leading to restlessness, sweating and tremors)
9 days ago- Started talking and laughing to himself, decreased food intake, unable to recognize family members, has short term memory loss.
Anatomical localization: There are lesions in the central nervous system.
Etiology: Since the Patient has a history of consumption of alcohol, this will lead to a deficiency in thiamine. A thiamine deficiency gives rise to Wernicke’s Encephalopathy, which is the presence of neurological symptoms caused by biochemical lesions of the central nervous system after exhaustion of B-vitamin reserves,
2) intervention
a) IVF NS and RL @150ml/hr
- Normal saline and ringer lactate solutions are both crystalloid fluids. NS contains 154 mM Na+ and Cl-, with an average pH of 5.0 and osmolarity of 308 mOsm/L. LR solution has an average pH of 6.5, is hypo-osmolar (272 mOsm/L), and has similar electrolytes (130 mM Na+, 109 mM Cl-, 28 mM lactate, etc.) to plasma.
b) Inj. 1amp Thiamine in 100ml NS, TID
Thiamine is given in patients that are chronic alcoholics, due to the pathology which causes the thiamine levels in the body are deficient. Thiamine is required in the breakdown of glucose.
c) Inj. Lorazepam
Lorazepam is mostly given to reduce the anxiety the patient feels.
- According to studies, Lorazepam has a 50% better result rate in reducing the patient’s anxiety than a placebo.
d) Tab Pregabalin 75mg/PO/ BD
- MOA: Although the mechanism of action has not been fully elucidated, studies involving structurally related drugs suggest that presynaptic binding of pregabalin to voltage-gated calcium channels is key to the antiseizure and antinociceptive effects observed in animal models.
- Indication: Pregabalin is indicated for the management of neuropathic pain associated with diabetic peripheral neuropathy, postherpetic neuralgia etc and as adjunctive therapy for the treatment of partial-onset seizures in patients.
e) Lactulose 30ml/PO/BD
MOA: Lactulose is a synthetic disaccharide derivative of lactose. Saccharolytic bacteria present in the large intestine subsequently break the substance down into organic acids like lactic acid. Such resultant volatile fatty acid metabolites, in combination with hydrogen and methane that is also generated consequently increase intraluminal gas formation, gut motility, and elicit an osmotic effect that facilitates an increase in the water content of stool as well as associated stool softening. All of these actions ultimately assist in facilitating and increasing the frequency of bowel movements in patients experiencing constipation.
Indication: Lactulose is also employed as an adjunct to protein restriction and supportive therapy for the prevention and treatment of portal-systemic encephalopathy (PSE), including both the hepatic pre-coma and coma variations.
f) Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
- MOA: Supplemental potassium in the form of high potassium food or potassium chloride may be able to restore normal potassium levels.
- Indication: For use as an electrolyte replenisher and in the treatment of hypokalemia.
3) Seizures: Repeated alcohol intake and withdrawal is termed as kindling. Kindling is a process whereby there can be small chemical and electrical stimuli which can precipitate the seizure activity.
Memory Loss: Alcohol may have a direct neurotoxic effect on cortical neurons, but much of the damage may be secondary to a pre-existing pathology caused by thiamine deficiency
. With the continuous use of alcohol, there is a constant decrease in the levels on thiamine in the body, which gives rise to delayed neurological symptoms.
4) A chronic alcoholic has a depleted supply of thiamine in the body, due to poor diet, which can give rise to neurological symptoms, such as Wernicke Encephalopathy. To prevent some of the symptoms, thiamine is given to replenish the supply of the patient.
5). Chronic alcohol consumption induces profound injury in several organs that may affect and aggravate the effect of ethanol on the kidney.
Ethanol itself markedly induces the expression of the microsomal ethanol oxidation system, producing reactive oxygen species as a byproduct. Increased gastrointestinal permeability and endotoxin load may lead to alcoholic steatohepatitis resulting in excessive immunoglobulin A (IgA) load. IgA deposits may accumulate in the kidney, leading to glomerulopathy.
Renal microcirculatory changes in advanced liver cirrhosis leads to hepatorenal syndrome. Alcohol-induced skeletal muscle damage leads to excessive amounts of circulating myoglobin, causing renal tubular injury because of increased oxidative stress.
6) The probable cause for normocytic anemia is kidney disease.
7) Yes, chronic alcoholism could have aggravated the formation on the foot ulcer. In the case of a chronic alcoholic, there is a depression in the immune system, the same way it is for diabetics. This can also lead to alcoholic neuropathy. Alcoholic neuropathy involves coasting caused by damage to nerves that results from long term excessive drinking of alcohol and is characterized by spontaneous burning pain, hyperalgesia, and allodynia. Chronic presentation will increase the chances of foot ulcer formation and also increase the time of recovery.
References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513691/#:~:text=One%20possible%20mechanism%20is%20oxidative,tissue%20injury%20and%20increase%20inflammation
Neurology case b
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Did the patients history of denovo HTN contribute to his current condition?
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
1) The symptoms started a week ago when he experienced giddiness which reduced after that but then occurred again after 3 days following alcohol consumption. This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus. 2 days ago he came to the OPD due to slurring of speech and deviated mouth. The anatomical location is in right inferior cerebellar hemisphere. Primary etiology is due to hypertension.
2) :Ecosprin 75 mg Tablet is an anti-platelet medicine that contains acetylsalicylic acid (also known as Aspirin). It is used to prevent blood clot formation within the body. This tablet is also used to prevent heart attacks, stroke and heart-related chest pain (angina). Zofer is used for the associated vomiting. Statins are given to reduce the cholesterol. Clopidogrel prevents clot formation. Vertin Tablet is used to prevent and treat a disorder of the inner ear known as Ménière's disease. The symptoms include dizziness (vertigo), ringing in the ears (tinnitus), and loss of hearing, probably caused by fluid in the ear. This medicine helps relieve the symptoms by reducing the amount of fluid.
3) :Blood vessels damaged by high blood pressure can narrow, rupture or leak. High blood pressure can also cause blood clots to form in the arteries leading to your brain, blocking blood flow and potentially causing a stroke
4) Drinking may, in fact, increase the risk of hemorrhagic stroke. This is more apparent when looking at the heavy drinking category
(neurology)case c
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
Questions
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
1) The probable cause for patient's condition of is due to Recurrent hypokalemic paralysis.
She also is diagnosed with cervical spondylosis which explains the chest heaviness, dyspnea, palpitations.
2) recurrence of hypokalemia: probable cause is due to periodic hypokalemic paralysis or genetic (autosomal inherited). (Also-- associated with hypothyroidism).
The risk factors may be :
-Alcohol use (excessive)
-Chronic kidney disease.
-Diabetic ketoacidosis.
-Diarrhea.
-Diuretics (water retention relievers)
-Excessive laxative use.
-Excessive sweating.
-Folic acid deficiency.
-Drug toxicity- (THPP)
3)ECG changes in hypokalemia:
ECG changes include :
-flattening and inversion of T waves in mild hypokalemia,
-followed by Q-T interval prolongation,
-apparent long QT intervals due to merging of the T and U wave
-increased amplitude and width of P wave,
-visible U wave and mild ST depression4 in more severe hypokalemia.
-Severe hypokalemia can also result in arrhythmias such as Torsades de points and ventricular tachycardia.
Neurology case D
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
1) Stroke is the most common cause of seizures in the elderly.
Stroke is of two types:
· Hemorrhagic stroke- this occurs as a result of bleeding within or around the brain.
· Ischemic stroke- this occurs as a result of blood clot or a lack of blood flow to the brain.
People who’ve had a hemorrhagic stroke are more likely to have seizures after a stroke than those who’ve had an ischemic stroke.
Seizures following a stroke (post seizure stroke) are of 2 types:
· Early onset seizures have peak within 24 hours after stroke.
· Late onset seizures occur after 2 week of stroke onset, peak within 6-12 months after the stroke has a higher rate of recurrence
Epilepsy is a condition characterised by recurrent episodes of seizures
Pathogenesis of seizures following stroke-
Early onset seizures after ischaemic strokes are due to an increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation.
Late onset seizures are due to glottic scarring and are associated with the persistent changes in neuronal excitability
2) In focal aware seizures (FAS), previously called simple partial seizures, the person is conscious (aware and alert) and will usually know that something is happening and will remember the seizure afterwards.Epileptic seizures can cause dynamic, reversible changes in brain function and are often associated with loss of consciousness.
References: https://www.scielo.br/j/jbn/a/MzmnPh7bHgnk4b4J9CmjsfN/?lang=en
https://www.medscape.com/answers/242008-160506/which-ecg-findings-suggest-hypokalemia-low-potassium-level
https://pubmed.ncbi.nlm.nih.gov/23776877/
Neurology case e
1)What could have been the reason for this patient to develop ataxia in the past 1 year?
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses
1) . This patient has a history of alcohol abuse for the past three years. Excessive alcohol consumption can be a major risk factor for development of cerebellar dysfunction or cerebellar ataxia.
A potential mechanism for this is alteration in GABA-A receptor dependent neurotransmission. Ethanol is shown to disrupt molecular events at the mossy fibre-granule cell-golgi cell synaptic site and the granule cell fibre-Purkinje cell synaptic site, which is mainly responsible for ethanol induced cerebellar ataxia.
Another mechanism is the relation between age related effect of ethanol on the endoplasmic reticulum of purkinje cells of dendrite causing dendritic regression, and the effect of ethanol withdrawal that causes mitochondrial damage in the cerebellum.
Ethanol also causes neuroinflammation and neurotoxicity in the cerebellum.
These can all affect the cerebellum, which is the motor coordination centre of the central nervous system, and also involved in cognitive processing and sensory discrimination. These can all result in altered hand movements, impaired postural stability and balance, loss of fine movements etc
2) stroke, Chronic alcoholics have decreased concentrations of liver-produced coagulation factors and platelet abnormalities that predispose them to hemorrhagic stroke.
Neurology case f
1.Does the patient's history of road traffic accident have any role in his present condition?
2.What are warning signs of CVA?
3.What is the drug rationale in CVA?
4. Does alcohol has any role in his attack?
5.Does his lipid profile has any role for his attack??
1) The road traffic accident could be implicated in CVA but not in this case scenario as the accident was 4 years ago.
2) :The five warning signs of stroke are:
Sudden onset of weakness or numbness on one side of the body.
Sudden speech difficulty or confusion.
Sudden difficulty seeing in one or both eyes.
Sudden onset of dizziness, trouble walking or loss of balance.
Sudden, severe headache with no known cause.
3). Ecosprin 75 mg Tablet is an antiplatelet medicine that contains acetylsalicylic acid (also known as Aspirin). It is used to prevent blood clot formation within the body. This tablet is also used to prevent heart attacks, stroke and heart-related chest pain (angina). Atorvastatin is also given to reduce the cholesterol.
4) Epidemiological evidence indicates that recent heavy alcohol consumption increases the risk for all major types of stroke, whereas light-to-moderate alcohol intake is associated with a decreased risk of ischemic stroke. Although heavy drinking elevates blood pressure, there is no firm evidence to indicate that alcohol consumption causes the formation of aneurysms, microaneurysms or other lesions in human arteries. Alcohol has been reported to precipitate vasoconstriction and rupture of small cerebral arteries in experimental animals. Alcohol-induced neck trauma has been shown to precipitate traumatic strokes, and alcohol-induced cardiac arrhythmias have been observed in patients with embolic brain infarction. The effects of alcohol on hemostasis, fibrinolysis and blood clotting are variable and could either prevent or promote the occurrence of strokes. The antiatherogenic effects of regular light-to-moderate alcohol consumption could be mediated by inhibition of low-density lipoprotein oxidation, and by elevated estrogen levels.
5)The patients lipid profile seems to be normal except for low HDL.
Neurology case g
1)What is myelopathy hand ?
2)What is finger escape ?
3)What is Hoffman’s reflex?
1) . A characteristic dysfunction of the hand observed in various cervical spinal disorders, there is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)It is one of the signs in cervical cord damage, in particular cervical myelopathy.
When patient holds fingers extended and adducted, the small finger spontaneously abducts due to weakness of intrinsic muscle.
It is a component of Wartenberg’s sign-consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.
This commonly results from weakness of the ulnar nerve innervated intrinsic hand muscles particularly palmar interosseus muscle.
3) Hoffman's sign or reflex is a test that doctors use to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition.
Neurology case h
1) What can be the cause of her condition ?
2) What are the risk factors for cortical vein thrombosis?
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
4) What drug was used in suspicion of cortical venous sinus thrombosis?
1) the patient has iron deficiency anaemia so it is possible that it caused her condition.
2) Problems with the way their blood forms clots.
Sickle cell anemia.
Chronic hemolytic anemia.
Beta-thalassemia major.
Heart disease — either congenital (you're born with it) or acquired (you develop it)
Iron deficiency.
Certain infections.
Dehydration.
3)The postictal state is a period that begins when a seizure subsides and ends when the patient returns to baseline. It typically lasts between 5 and 30 minutes and is characterised by disorienting symptoms such as confusion, drowsiness, hypertension, headache, nausea, etc
4) Heparin should be considered seriously in the management of cerebral venous thrombosis (CVT), with subsequent conversion to warfarin as maintenance therapy suggested. Subcutaneous low ̶ molecular-weight heparin (Lovenox) also has been used in patients with venous sinus thrombosis. Thrombolytic therapy may be effective in CVT, but all studies so far describe its use only with local instillation by micro-catheter or direct instillation at the time of surgical thrombectomy
Cardiology case a
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
2.Why haven't we done pericardiocenetis in this pateint?
3.What are the risk factors for development of heart failure in the patient?
4.What could be the cause for hypotension in this patient?
1) Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure. The heart muscle does not contract effectively, and therefore less oxygen-rich blood is pumped out to the body.
2)
Pericardiocentesis is a procedure done to remove fluid that has built up in the sac around the heart (pericardium).
It's done using a needle and small catheter to drain excess fluid.
There are 3 approaches for needle entry - left parasternal, subxyphiod approach, left apical approach. All these require a lot of precision as they might damage the surrounding pleura, diaphragm , liver.
Pericardial effusion is mild - moderate in this patient , so symptomatic treatment was given rather than opting for an invasive procedure like pericardiocentesis which requires a lot of precision.
Risks of pericardiocentesis include- Puncturing the heart, which may require surgery to repair, Puncturing the liver, Excess bleeding, which might compress the heart and affect its normal function, Air in the chest cavity, Infection etc. if the procedure is not done properly
3) The patient is old, and has a history of smoking and is also a known case of hypertension. These could've led to the development of heart failure in this patient
4)
Hypotension in this patient could be due to combination of pericardial effusion and use of diuretic LASIX (furosemide).
The pumping ability of the heart in this patient is compromised already. Along with this he is on a loop diuretic (causing sodium, potassium and chloride loss in the urine) and is on anti hypertensive medication (Telma 40 mg), along with fluid restriction. All these factors might result in Hypovolemia and thereby Hypotension
Cardiology case b
1.What are the possible causes for heart failure in this patient?
2.what is the reason for anaemia in this case?
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
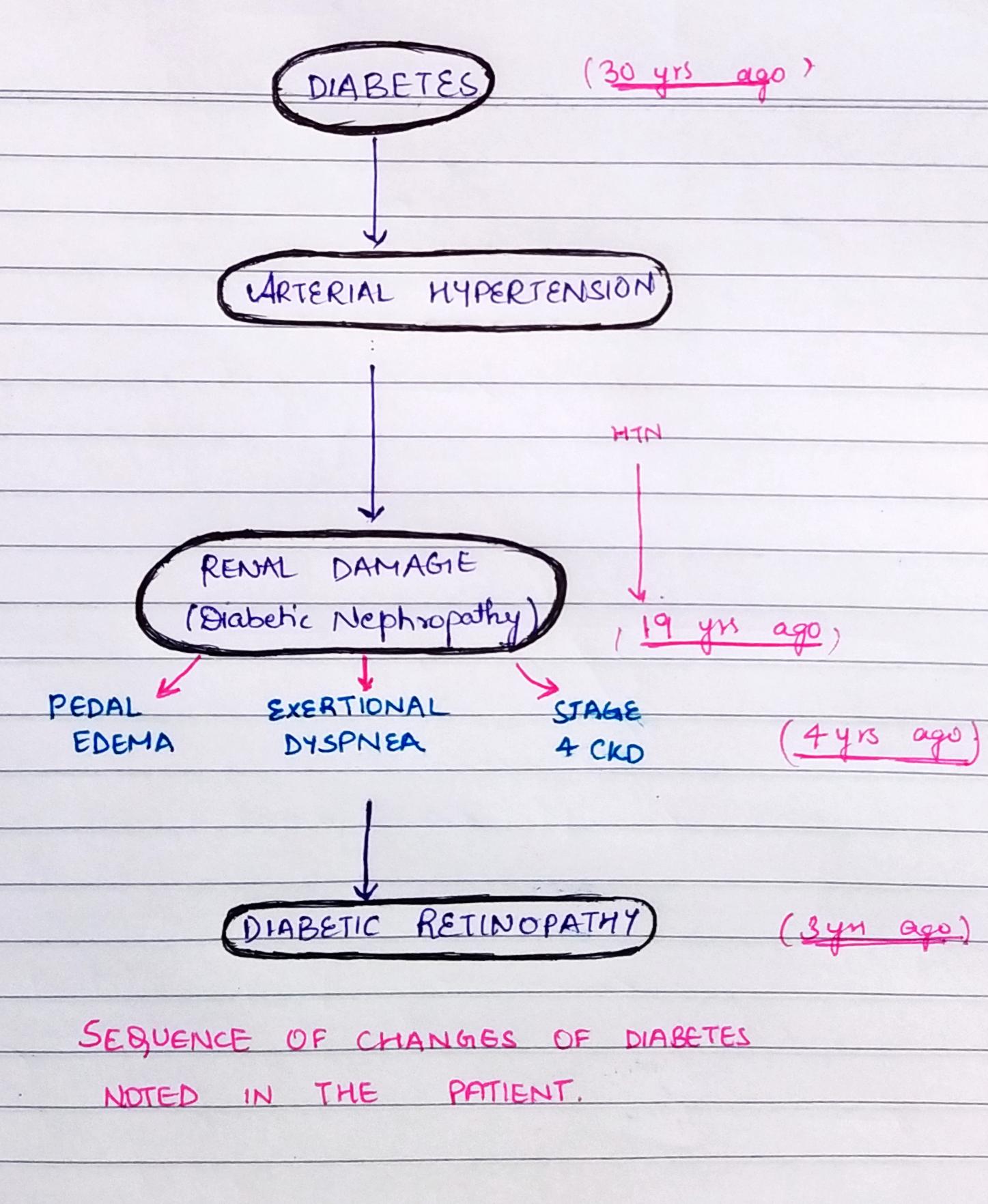
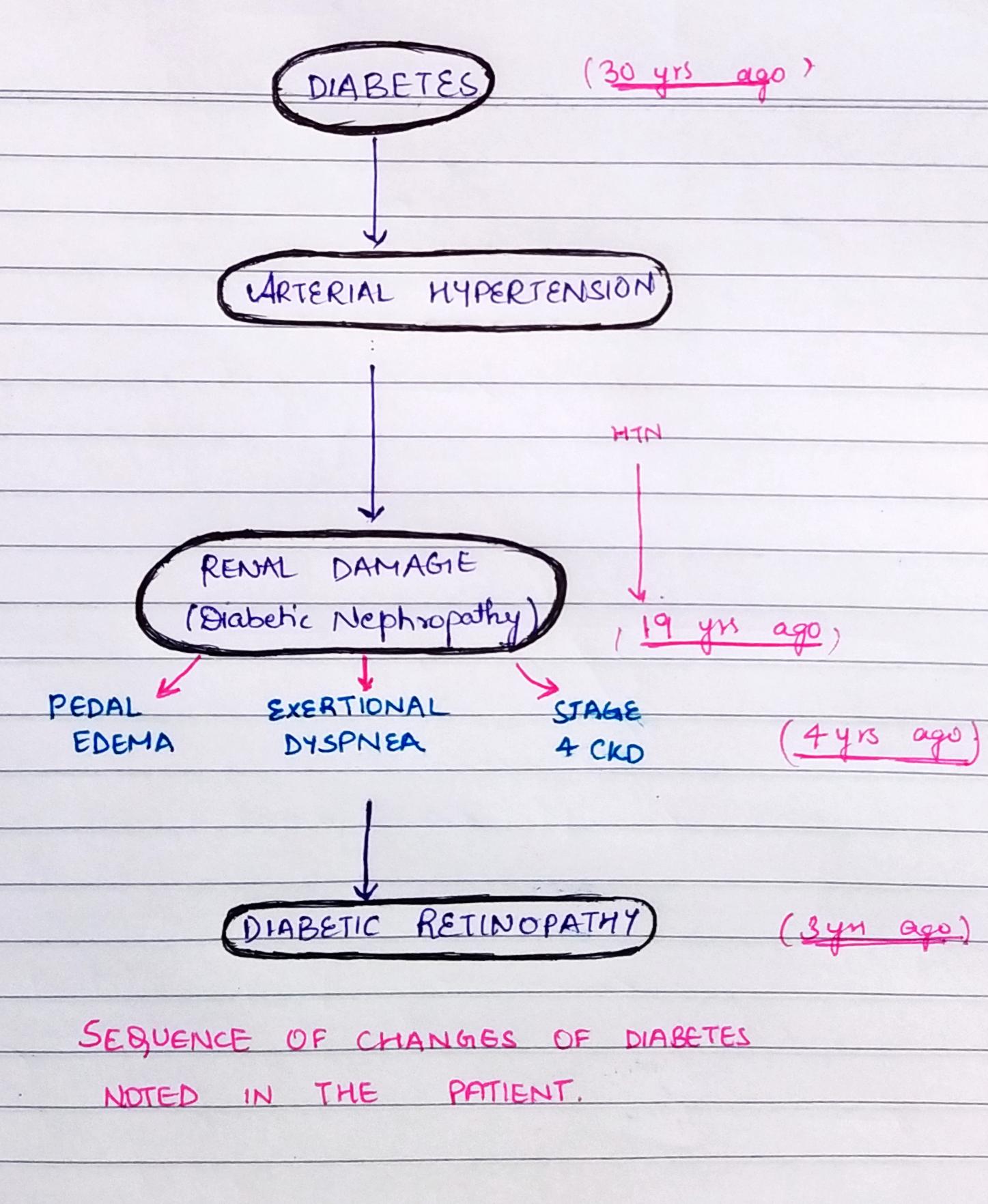
4. What sequence of stages of diabetes has been noted in this patient?
1) patient is old and has a history of chronic alcoholism and is a known case of hypertension and diabetes mellitus and chronic kidney disease. The patient is also obese and has central truncal obesity. These could be responsible for his heart failure.
possible causes of heart failure :
Diabetic nephropathy causing renal damage due to which the optimal blood pressure is not maintained adding to the risk of heart failure
Hypertension.
Chronic renal disease.
The liver diseases are risk factors affecting the heart include complications of cirrhosis such as hepatopulmonary syndrome, portopulmonary hypertension, pericardial effusion, and cirrhotic cardiomyopathy. (The patient is chronic alcoholic since 30yrs)
2)anemia :
The major causes of anemia in CKD patients are iron and erythropoietin deficiencies and hyporesponsiveness to the actions of erythropoietin.
Liver disease - (chronic alcoholic) macrocytic anemia
3) possible cause for blebs :Could be because of diabetes -bacterial infections, fungal infections, and itching. Other skin problems happen mostly or only to people with diabetes.
The healing process in diabetics is slowed down.
High blood glucose impairs the function of white blood cells. White blood cells are central to the role of the immune system. When white blood cells are unable to function correctly, the body is less able to fight bacteria and close wounds.
4) 
Cardiology case c
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
4) What are the risk factors for atherosclerosis in this patient?
5) Why was the patient asked to get those APTT, INR tests for review?
1)Timeline of the patient is as follows-
· 1 year ago- History of shortness of breath (Grade II- SOB on exertion); He visited the hospital where he was diagnosed to be hypertensive (on medication)
· 2 days ago- Patient was apparently asymptomatic 2 days ago when he developed Shortness of breath Grade II (on exertion) which progressed to Grade IV (at rest) for which he visited local RMP and was referred to our hospital. Patient also complains of decreased urine output since 2 days.
· Present day- Patient came to the hospital with SOB grade IV (on rest) and anuria for the past one day.
Anatomical Location- Patient has an issue that was localized as an issue in the cardiac region.
Etiology- Congestive heart failure is a chronic progressive condition that affects the pumping power of the cardiac muscle. It occurs if the heart cannot pump (systolic) or fill (diastolic) adequately. Loss of atrial contraction and left atrial dilation in this case cause stasis of blood in the left atrium and may lead to thrombus formation in the left atrial appendage. This predisposes to stroke and other forms of systemic embolism.
2)INJ. Dobutamine-
MOA- It is a synthetic catecholamine, that acts on B1, B2 and alpha 1 receptors.
Indications- It is a potent inotropic agent but only causes a slight increase in heart rate. It is given to patients with acute heart failure as iv infusion. 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg in this case.
b) TAB. Digoxin-
MOA- It acts on the digitalis receptor and inhibits NA-K-ATPase, thus increasing cardiac output.
Indications- Digitalis is used in patients with low output failure especially when associated with atrial fibrillation, as indicated in this case.
c) INJ. Unfractionated Heparin 5000-
MOA- At low concentration, heparin selectively inhibits the conversion of prothrombin to thrombin, thus preventing thrombus formation. High dose heparin has antiplatelet action and prolongs bleeding time.
Indications- Patient had a biatrial thrombus and in this case it was used to prevent further thrombus formation.
d) TAB. Carvediol 3.125mg BD
MOA- It blocks B1, B2, Alpha 1 adrenergic receptors and no intrinsic sympathomimetic activity.
Indications- Used as a long term drug to reduce mortality in patients with congestive heart failure.
e) TAB. Acetyl cysteine 600mg PO TID
f) TAB. Acitrom 2mg OD
MOA- It is an anticoagulant that functions as a vitamin K antagonist.
Indications- oral anticoagulant which helps to prevent formation of harmful blood clots in the legs, lungs, brain and heart. It is used for deep vein thrombosis, pulmonary embolism and stroke prevention.
g) TAB. Cardivas 3.125mg PO/BD
MOA- It is carvediol. It blocks B1, B2, Alpha 1 adrenergic receptors and no intrinsic sympathomimetic activity.
Indications- Used as a long term drug to reduce mortality in patients with congestive heart failure.
h) TAB. Dytor 10mg PO/OD
MOA- It is torsemide, a loop high ceiling diuretic. It acts on the thick ascending limb of the loop of henle, increases Na, K and Cl excretion in the urine.
Indications- preferred in cases of hypertension associated with CCF and renal failure.
i) TAB Pan D 40mg PO/OD
MOA- It is a combination of domperidone and pantaprazol. It is a proton pump inhibitor and helps decrease acid production in the stomach.
Indications- used to treat gastroesophageal reflux disease (Acid reflux) and peptic ulcer disease by relieving the symptoms of acidity such as indigestion, heartburn, stomach pain, or irritation.
j) TAB. Taxim 200mg PO/OD
MOA- It is cefixime. They are beta-lactam antibiotics that inhibit synthesis of bacterial cell wall and produce a bactericidal effect.
Indications- Given mainly to prevent development of bacterial infections.
k) INJ. Thiamine 100mg in 50ml NS IV/TID
It is vitamin B1. It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
l) INJ. HAI S.C 8U-8U-6U
Insulin given in this case to treat the patients denovo diabetes mellitus.
3) The term cardio renal syndrome (CRS) refers to a condition in which either renal impairment occurs as a result of cardiac dysfunction, or heart structure and function are negatively affected by renal disorders. The damage/dysfunction can be produced in either the heart or the kidney by an acute or chronic disease of the other organ, or abnormal heart and kidney functions occur simultaneously as a result of a systemic disease
4) : Risk factors for atherosclerosis, include:
High cholesterol and triglyceride levels.
High blood pressure.
Smoking.
Type 1 diabetes.
Obesity.
Physical inactivity.
High saturated fat diet.
5) APTT measures heparin levels while INR is a measure of warfarin and they help to prevent and check out for toxicities or excess of these anticoagulants so that the patient won't bleed out.
Cardiology case d
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What are the indications and contraindications for PCI?
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
1) Timeline of events-
- 12 years ago- Diagnosed with type 2 diabetes mellitus (on medication)
- Last 1 year- Heart burn like episodes since, relieved without medication
- 7 months ago- Diagnosed with pulmonary TB; Completed full course of treatment; presently sputum negative.
- Past 6 months - Hypertension diagnosis (on medication)
- Since half an hour- Shortness of breath, Grade IV (SOB even at rest)
Anatomical localisation - Cardiovascular system
Etiology- The patient is both Hypertensive and diabetic, both these conditions can cause atherosclerosis (there is build up of fatty and fibrous material inside the wall of arteries)
2) Met XL 25 tablet is used to treat high blood pressure mainly, along with certain heart conditions such as angina (chest pain) and heart failure. belongs to a group of medicines called long-acting beta-blocker. Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a nonsurgical technique for treating obstructive coronary artery disease, including unstable angina, acute myocardial infarction (MI), and multi vessel coronary artery disease (CAD).
3)Indications:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
Contraindications:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
An artery with a diameter of <1.5 mm
4)Although PCI is generally a safe procedure , it might cause serious certain complications like
Bleeding
Blood vessel damage
Allergic reaction to the contrast dye used
Arrhythmias
Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it. Research on over-testing and over-treatment is important as they are more harmful than useful.
Overtreatment: the worst consequence of overdiagnosis is overtreatment of an indolent lesion or disease which is unlikely to have any benefit for the patient
over diagnosis in some non-neoplastic conditions leads to over-prescription and over medicalization, resulting in many undesirable and sometimes dangerous side effects
Cardiology case e
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
1) Patient was apparently asymptomatic 3 days back and then he developed mild chest pain in the right side of the chest. The problem is in the heart of the patient. Elevations lead 2 and 3 and AVF indicate the problem is in inferior area, probably right coronary artery(90%).
Causes:
Atherosclerosis – Also known as coronary artery disease, this condition is the most common cause of heart attacks and occurs when the buildup of fat, cholesterol, and other substances forms plaque on the walls of the coronary arteries
Coronary artery spasm – A rare cause of blockage, spasms of the coronary arteries can cause them to become temporarily constricted.
Coronary artery tear – Also known as a spontaneous coronary artery dissection, a tear in a coronary artery can prevent blood from reaching the heart and cause a heart attack.
2) Daily low-dose aspirin is a blood thinning medicine. Aspirin is also known as acetylsalicylic acid. Low-dose aspirin helps to prevent heart attacks and strokes in people at high risk of them. Atorvastatin belongs to a group of medicines called statins. It's used to lower cholesterol if you've been diagnosed with high blood cholesterol. It's also taken to prevent heart disease, including heart attacks and strokes. Clopidogrel is an anti platelet medicine. It prevents platelets (a type of blood cell) from sticking together and forming a dangerous blood clot. Taking clopidogrel helps prevent blood clots if you have an increased risk of having them. Inj HAI relaxes and dilates (expands) blood vessels resulting in lowered blood pressure. It is used to treat hypertension (high blood pressure). PTCA, or percutaneous trans luminal coronary angioplasty, is a minimally invasive procedure that opens blocked coronary arteries to improve blood flow to the heart muscle.
3) : In this patient the PTCA was unnecessary. Indications of PTCA depend on various factors. Patients with stable angina symptoms unresponsive to maximal medical therapy will benefit from PCI. It helps provide relief of persistent angina symptoms despite maximal medical therapy. Emergency PTCA is indicated for acute ST-elevation myocardial infarction (STEMI) suggesting 100% occlusion of the coronary artery. With acute STEMI, patients are taken directly to lab immediately upon presentation to help prevent further myocardial muscle damage. In non-ST-elevation myocardial infarction (NSTEMI), or unstable angina, (known as acute coronary syndromes), patients are taken to cardiac cath lab within 24 to 48 hours.
Cardiology Case f
1.How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
2. What is the rationale of using torsemide in this patient?
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
1) The patient presented with rapid breathing, which is an indicator of cardiogenic shock, if the patient also presents along with other signs such as cold, clammy extremities.
In cardiogenic shock, there is hypovolemia, which causes reduced perfusion to major organs in the body. When there is decreased perfusion, the body slows starts shutting down. To halt this process, iv fluids are given rapidly to continue the perfusion of fluids at the normal rate. Fluid resuscitation helps restore lost blood volume, regain tissue perfusion, and reduce mortality.
When this patient was given fluids, the perfusion returns to normal which helps abate the shortness of breath.
2)In patients who have cardiorenal syndrome, there is a renal dysfunction along with cardiac abnormalities. In such patients there is a volume overload and heart failure, the combination of which causes increased pulmonary artery or central venous pressure with low systemic pressure that may lead to a severe compromise of the net renal perfusion pressure.
Furosemide is a commonly used diuretic to treat volume overload state in heart failure, yet it is particularly prone to the problem of diuretic resistance because of its particular pharmacokinetics. Alternatives to furosemide, such as torsemide, have been shown to have a slight advantage in selected studies because of somewhat more favourable pharmacokinetics, such as longer half life and increased bioavailability of the drug.
3) Patients with cardiorenal syndrome are known to have systemic inflammation which can be drawn parallel to end stage kidney disease. Here there is an inflammation of monocytes and other inflammatory cells. This puts the patient in a immune suppressive state.
Due to this state, to reduce the chances of infection, as a prophylactic measure, ceftriaxone might have been started.
Gastroenterology & pulmonology case a
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1) Patient was apparently asymptomatic 5 yrs back when he had pain abdomen & vomiting. He was symptom free for nearly 3 yrs. Last binge of alcohol was 1 week back following which he again had pain abdomen & vomiting from 1 week and fever from 4 days. Then he developed constipation since 4 days and passing flatus. patient also had burning micturition since 4 days. The problem can be localised to pancreas. The cause of pancreatitis here may be attributed to alcohol.
2)
Ans: (1) ING. MEROPENAM ; TID for 7 days
* Meropenem ( broad spectrum Carbepenem ) an antibiotic.
(2) ING. METROGYL 500 mg IV TID for 5 days
* inj. Metrogyl has METRONIDAZOLE
( Nitroimidazole drug ) an antibiotic
(3) ING. AMIKACIN 500 mg IV BD for 5days
* It is an Aminoglycoside antibiotic
## Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
4) TPN ( Total Parenteral Nutrition )
* Method of feeding that by passes gastrointestinal tract
* Fluids are given to vein , it provides most of the nutrients body needs.
* TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
* Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD
* Inj. Pantop has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD
* It is an opioid analgesic, given to relieve pain.
Case b
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
2) Name possible reasons why the patient has developed a state of hyperglycemia.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
4) What is the line of treatment in this patient?
1) (1)cause of dyspnea :is due to pleural effusion.
Activated proteolytic enzymes and cytokines, released by the inflamed pancreas not only digest pancreatic and peripancreatic tissues but also activate other enzymes such as elastase and phospholipase A2 . The active enzymes and cytokines then digest cellular membranes and cause proteolysis, edema, interstitial hemorrhage, vascular damage, coagulation necrosis, fat necrosis, and parenchymal cell necrosis.
Cellular injury and death result in the liberation of bradykinin peptides, vasoactive substances, and histamine that can produce vasodilation, increased vascular permeability, and edema with profound effects on many organs. The systemic inflammatory response syndrome (SIRS) and acute respiratory distress syndrome (ARDS), as well as multiorgan failure, may occur as a result of this cascade of local and distant effects.
(2) State of hyperglycemia
Insulin resistance in ALD develops from alcohol's effects on hepatic and non-hepatic tissues and may be exacerbated by the steatogenic effects of overnutrition on the liver. The combined hepatic effect of alcohol overconsumption and overnutrition.
Insulin resistance impairs glucose
utilization by insulin-sensitive tissues and increases hepatic glucose
output; both effects contribute to the hyperglycemia. Increased hepatic
glucose output predominantly accounts for increased FPG levels,
whereas decreased peripheral glucose utilization results in postpran-dial hyperglycemia.
(3) Elevated LFTs and alcohol markers
The elevation of the enzyme activity in the serum primarily reflects its increased rate of enterance into serum caused due to (i) from damaged liver cells.(AST/ALT ratio) (ii) cholestasis (increased AST,GGT, 5'nucleotidase).
A ratio >3:1 is highly suggestive of alcoholic liver disease. The AST in alcoholic liver disease is rarely >300 IU/L, and the ALT is often normal. A low level of ALT in the serum is due to an alcohol-induced deficiency of pyridoxal phosphate.
Of all liver enzymes, GGT is considered to be the most sensitive biomarker of alcohol consumption.
(4) line of treatment:
Investigations:24 hour urinary protein,
Fasting and Post prandial Blood glucose,
HbA1c,
USG guided pleural tapping.
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
.GRBS charting 6th hourly
. BP charting 8th hourly
References: https://www.ncbi.nlm.nih.gov/books/NBK537191/#:~:text=Alcohol-induced%20pancreatitis%20occurs%20in,the%20mid-back%20or%20flanks.
Harrison's principles of internal medicine.
https://www.sciencedirect.com/topics/medicine-and-dentistry/liver-enzyme
Case c
1) what is the most probable diagnosis in this patient?
2) What was the cause of her death?
3) Does her NSAID abuse have something to do with her condition? How?
1) Intra peritoneal haemorrhage.
2): Haemorrhage is the loss of blood components from the cardiovascular system. Hemorrhagic shock occurs when this blood loss leads to inadequate tissue oxygenation. This could've caused her death.
3): Non steroidal anti-inflammatory drugs (NSAIDs) are effective anti-inflammatory and analgesic agents and are among the most commonly used classes of medications worldwide. However, their use has been associated with potentially serious dose-dependent gastrointestinal (GI) complications such as upper GI bleeding. This could've caused haemorrhage in her.
Nephrology case a
1. What could be the reason for his SOB ?
2. Why does he have intermittent episodes of drowsiness ?
3. Why did he complaint of fleshy mass like passage in his urine?
4. What are the complications of TURP that he may have had?
(1) Shortness of breath and chest tightness could be one of the signs of severe Post-TURP Syndrome.
( TURP syndrome which causes headaches, anxiety, confusion, dyspnoea, arrhythmia, hypotension and seizures and can be fatal if not treated). The symptoms of TURP are generally caused by an excessive fluid load in circulation.
It could also be because of complication of hydronephrosis due to electrolyte imbalance.i.e. Metabolic acidosis.
(2) Hyponatremia could be the cause of intermittent drowsiness.
Hyponatremia after transurethral resection of the prostate (TURP) or hysteroscopy is caused by absorption of irrigants, glycine, sorbitol, or mannitol, contained in nonconductive flushing solutions used for those procedures.
Symptoms of hyponatremia include lethargy, confusion, and fatigue.
In the most serious of cases of hydronephrosis, this can lead to loss of normal kidney function (kidney failure) which could be the cause of intermittent drowsiness due tiredness.
(3)pus cells and sloughing process: papillary necrosis. Immune responses to infections are generally balanced between bacterial clearance and tissue repair. However, in the bladder, the response prioritizes tissue repair
Researchers learned that the bladder’s intitial response emphasizes shedding cells from internal walls to reduce bacterial load
However, the sloughing process removes the thick plaque of cells that protects the bladder walls from salts and toxins in urine, which could be the cause of fleshy urine.
(4) TURP complications:
In this case is due to retrograde flow--> hydronephrosis---> papillary necrosis. Other causes: excessive bleedingrinary tract infections, retrograde flow , chronic urinary problems especially incontinence, prostate regrowth or scarring, with about 10 percent of men requiring further surgery within 5 years,impotence or erectile dysfunction,a split stream of urine caused by urethral narrowing,chronic prostatitis or inflammation of the prostate,allergic or abnormal reaction to anesthesia.
Nephrology case b
1.Why is the child excessively hyperactive without much of social etiquettes ?
2. Why doesn't the child have the excessive urge of urination at night time ?
3. How would you want to manage the patient to relieve him of his symptoms?
1)Attention deficit hyperactivity disorder (ADHD) is a mental health disorder that can cause above-normal levels of hyperactive and impulsive behaviours. People with ADHD may also have trouble focusing their attention on a single task or sitting still for long periods of time. Both adults and children can have ADHD.
2): Overactive bladder (OAB) represents a syndrome characterised by a myriad of lower urinary tract symptoms (LUTS) including urinary urgency, with or without urgency incontinence, usually with frequency and nocturia, in the absence of infection or other identifiable causes. The true nature of OAB remains elusive – myogenic changes, neurologic changes, urothelial changes and afferent sensitization have been hypothesized to contribute to the symptomatology of OAB. Here it the urge of urination could be psychosomatic due to which at night time he doesn't have it.
3.) Principles of treatment are to reduce urinary incontinence by changing patient behaviour and teaching continence skills. As OBS is a symptom complex, 'no treatment' is an acceptable choice for some patients and caregivers.
Infectious disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology)
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
1)In adults, the characteristic history is recurrent pneumonia, hemoptysis, and coughing after eating. In children, the features found in cases of congenital tracheoesophageal fistula, there is Frothy, white bubbles in the mouth, coughing or choking when feeding, vomiting, blue color of the skin (cyanosis), especially when the baby is feeding, difficulty breathing.
The physical findings are, in the presence of TEF, abdominal distention may occur secondary to collection of air in the stomach.
2). Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse.
There are chances that this patient can develop IRIS due to the patient being RVD positive. She is more susceptible to any infection and therefor prone to reinfection. To prevent IRIS, the most effective method is to involve the initiation of ART before immunosuppression is advanced. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL. Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
Infectious disease and hepatology
Case a
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?
What could be the cause in this patient ?
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
4.What are the indications for ultrasound guided aspiration of liver abscess ?
1) yes, Alcoholism is never an etiological factor for the formation of liver abscess.
From study it was proved that consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that are both amoebic as well as pyogenic liver abscess .
Alcohol has adverse effects on the liver.
2)Liver cirrhosis is therefore a strong risk factor for pyogenic liver abscesses and a risk factor for death. Loss of hepatic filter function, impaired immunity, and frequent abdominal infection and septicaemia in patients with cirrhosis are probably factors responsible.
3) right lobe has rich blood supply, therefore abscess is more common in the right lobe.
4) indications for USG guided aspiration.
-complicated diverticular abscess.
-Crohn's disease related abscess.
-complicated appendicitis with appendicular abscess.
-tuboovarian abscess.
-post-surgical fluid collections.
-hepatic abscess (e.g. amoebic or post-operative)
-renal abscess or retroperitoneal abscess.
-splenic abscess.
Case b
1) Cause of liver abcess in this patient ?
2) How do you approach this patient ?
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
4) Is there a way to confirmthe definitive diagnosis in this patient?
1) A liver abscess can develop from several different sources, including a blood infection, an abdominal infection, or an abdominal injury which has been become infected. The most common infecting bacteria include E coli, enterococcus, staphylococcus, and streptococcus. It could also be due to viral hepatitis.
2) INJECTION. ZOSTUM 1.5 gm IV BD (twice daily)
Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
* INJECTION. METROGYL 500mg IV TID ( thrice daily )
Metrogyl has the drug called METRONIDAZOLE [Antibiotic]: For amoebic cause
* INJECTION. OPTINEURIN 1amp in 100 ml NS( Nor
mal Saline) IV OD ( once daily)
Optineurin is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
* TAB. ULTRACET 1/2 QID( four times a day)
Ultracet is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN(analgesic and antipyretic) : Given for pain and fever
* TAB. DOLO 650 mg SOS (if needed) given for fever and pain.
3)
Ans: Considering the following factors:
1) Age of the patient (21) - young & gender- male ,
2) Single abscess,
3) Right lobe involvement,
The abscess is most likely to be AMOEBIC LIVER ABCESS.
Since we cannot take risk , we should however administer antibiotics also ( like in pyogenic liver abscess)
4)
Ans: It can be done by aspiration of the abscess and culture of the fluid from it. this lets us know the causative organism.
Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology)
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time ?
1)Fever since 10 days
Facial puffiness and periorbital edema since 4 days
Weakness of right upper limb and lower limb since 4 days
Altered sensorium since 2 days
The disease is localised to the frontal lobe of brain. Common causes of mucormycosis includes diabetes which the patient has.
2)The management of the patient was-
1. Inj. Liposomal amphotericin B
2. 200mg Iatraconazole was given as it was the only available drug which was adjusted to his creatinine clearance.
3. Deoxycholate was the required drug which was unavailable
Along with the above mentioned treatment for the patient managing others symptoms is also done by-
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
3) Mucormycosis may be being triggered by the use of steroids, which are life-saving drugs for severe and critically ill Covid-19 patients.
Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing.
Infectious disease ( COVID 19)
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
For this question that contains details of many of the hospitals Covid 19 patients documented over this month I have collected information adhering to the following
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe
3) Indicate for each patient, the day of Covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe Covid (for example, altered sensorium, hypotension etc).
I have compiled all the data collected in the form of an excel spreadsheet, so as to be able to draw a comparative analysis about the progression of disease and the outcome in various patients.
https://docs.google.com/document/d/e/2PACX-1vRhamXAWuJYe99RUJXxjhlvNcD3y0hZYTSLpKy6LAGZie-32LRrmJCDII-rSp-QLSVBCjhJUzTYZPm4/pub
Section 10
Elog making helped me alot in learning new cases and questions and discussions are very much helpful . As final year medical student in Covid we are in the fear of missing all clinical exposure that we had access to on the field. But Elog has helped esae that fear and the tension by enabling us to interact more and correlate different aspects of medicine .

