A 36 year old male with epigastric pain
-
This is an online e logbook to discuss our patients deidentified health data shared after taking her/guardian's signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs
This E log also reflects my patient centre’s online learning portfolio and valuable inputs on the comment box is welcome.
Case History
a 36 year old male , driver by occupation ,came to the casualty with
CHEIF COMPLAINTS OF -
complains
pain in the epigastric region since 8 days
HISTORY OF PRESENTING ILLNESS -patient was apparently asymptomatic 9 days back then he developed
pain in the epigastric region which was
sudden in onset ,
dragging type of pain and
non-radiating type , aggravated on sleeping in Lateral position relieved on medication. Tightness of the abdomen since 4 days
High grade
Fever since 9 days which was
sudden in onset associated
with chills and rigors and headache (frontal and occipital) . He developed shortness of breath since 5days (grade 2 ) constipation since 4 days and decrease in appetite.
complains of belching 2 to 3 times per day
He had similar episode previously in June 2021 with complaint of pain and distended abdomen.
no history of nausea vomiting , no h/o loose stool ,no history of past surgery
no history of jaundice previously
no history of gallstones,
PAST HISTORY - Similar history 6months back , not a known case of htn , dm , epilepsy , asthma , tb
no previous surgical history
no history of gallstones in the past
PERSONAL HISTORY :diet - mixed ,
appetite -decrease appetite ,
bowel movement - irregular since 3 days,
bladder movements - regular ,
addictions(alcohol and smoking) -
alcoholic in seven years takes at least 150 ml
occasional toddy user also since six months drinks 180 ml per day
brand used it is (royal stag or ib )180 ml per day is in six months
no history of smoking or chewing tobacco
FAMILY HISTORY -
not significant
GENERAL EXAMINATION -
patient is concious , coherent cooperative
no pallor , icterus Present - mild, clubbing , cyanosis , lymphadenopathy , edema
vitals -
8-1-22
temperature - afebrile
pulse rate - 97 bpm
blood pressure - 100 /70 mm of hg
respiratory rate - 22
spo2 - 98% at room air
SYSTEMIC EXAMINATION - cardiovascular system : s1 and s2 heard , no murmurs
respiratory system : bilateral air entry present ,normal vesicular breath sounds
central nervous system : nad
p/a -
Abdomen is slightly distended
Umbilicus central , inverted , all quadrants moving appropriately with respiration
No scars , engorged veins, no visible peristalsis or pulsations
pain in the epigastric region and
pain is more in the right iliac and lumbar region
no bruit’s , no gaurding, no rigidity
negative cullens sign and grey turners sign, no fox's sign
bowel sounds present
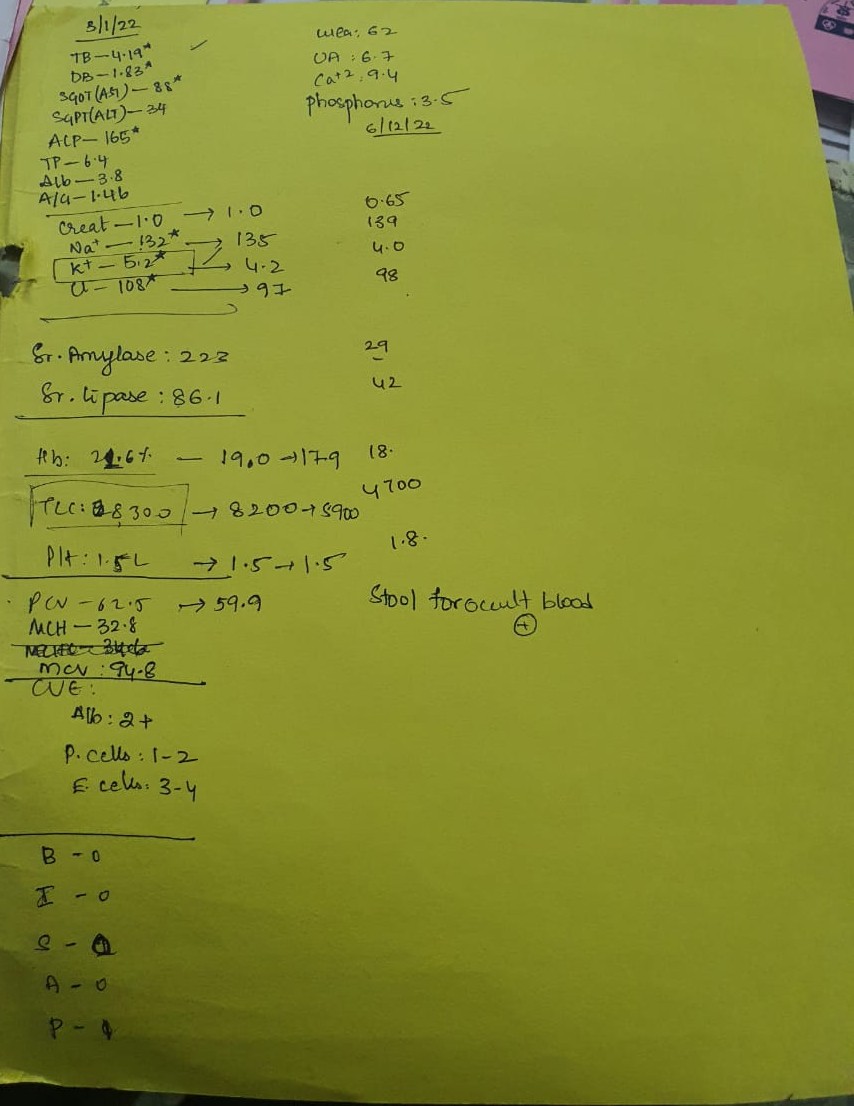
 INVESTIGATION -
INVESTIGATION -
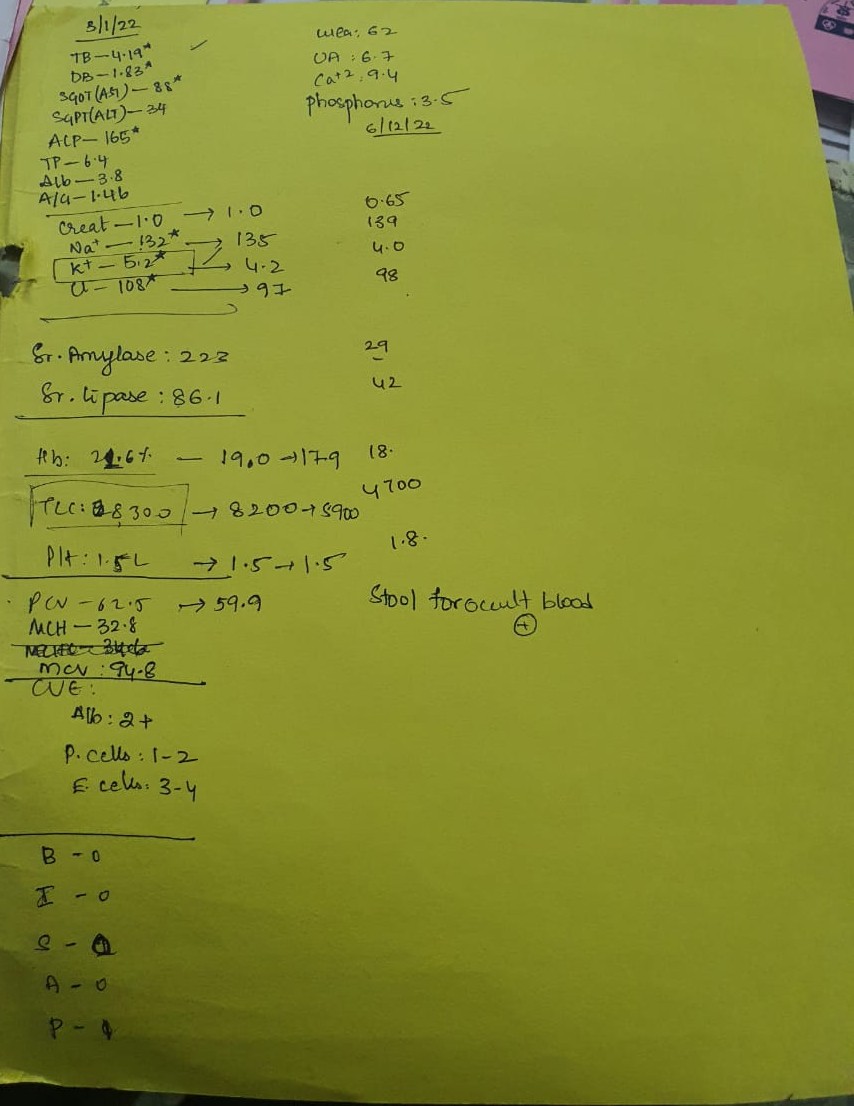
Elevated serum amylase and lipase
Stool for occult blood positive
HEMOGRAM: .jpg?alt=media&token=59bf3bda-2857-4ba2-89cc-dd6e9fccaf2f) CUE:
CUE:~2.jpg?alt=media&token=ed2330a4-9844-48c0-83a2-fe7a05b58566) RFT:
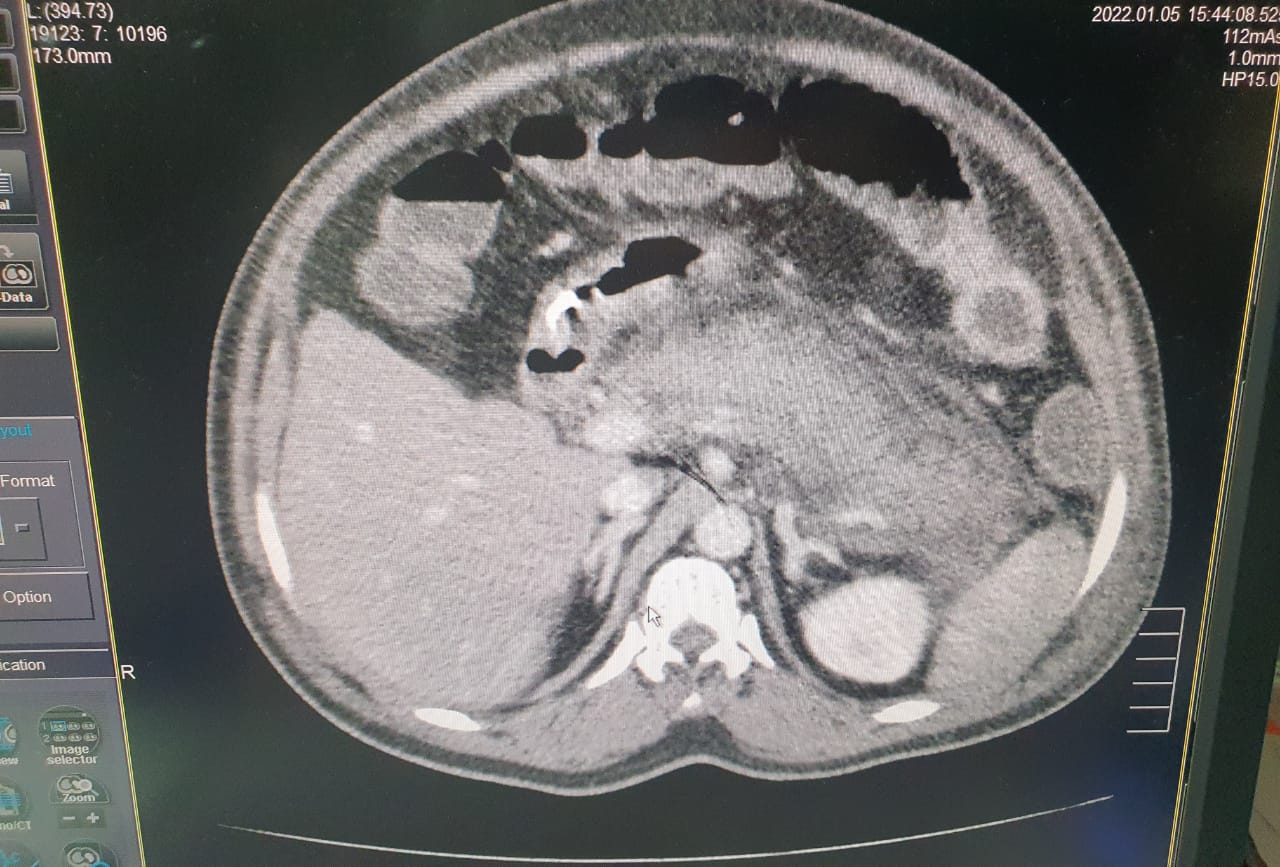
RFT:~2.jpg?alt=media&token=302c4101-c161-4419-8d2a-201a32e25769) CT scan
CT scan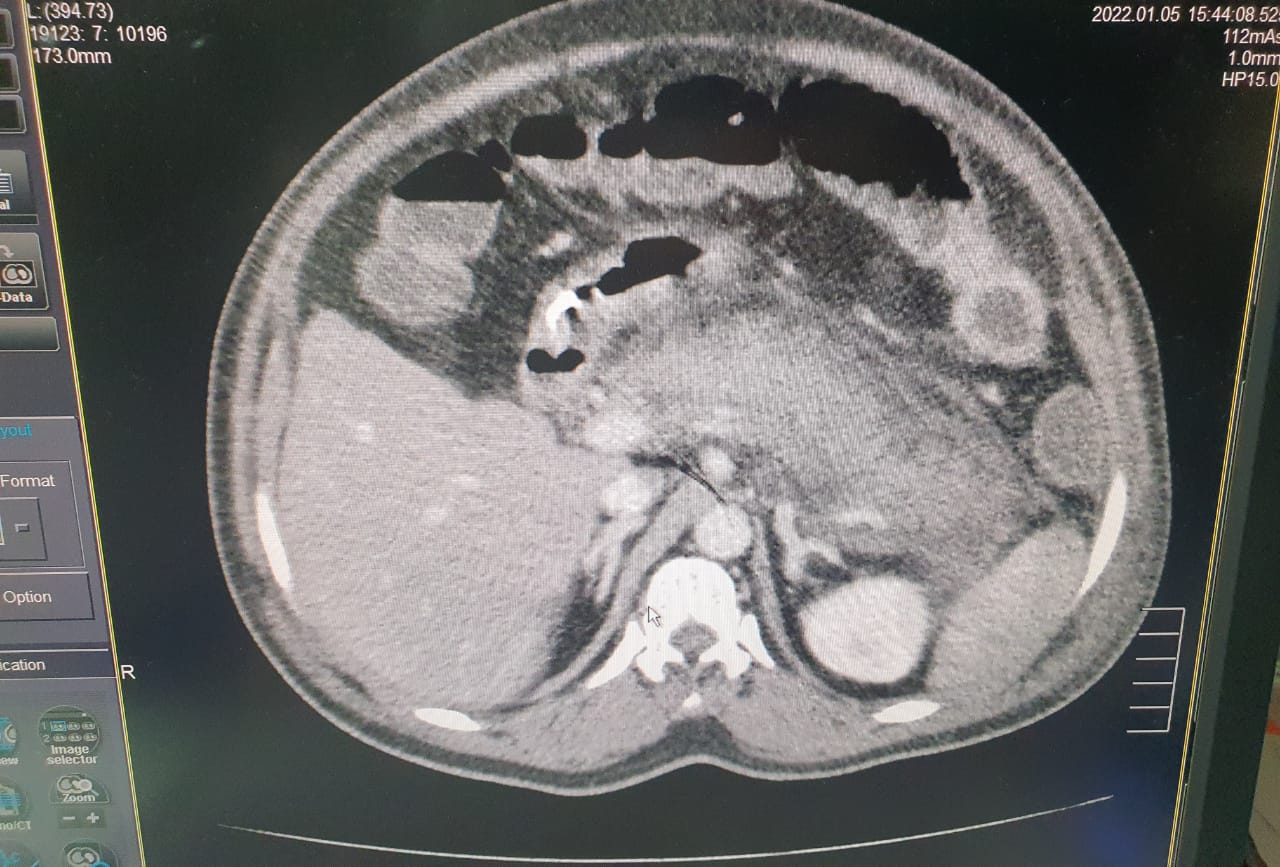

~2.jpg?alt=media&token=4f2b676c-e0b3-4bab-ace0-50c542a06534) COMPLETE URINE EXAMINATION
COMPLETE URINE EXAMINATION:
~2.jpg?alt=media&token=792db17a-82ba-4783-80bf-d60b26a7e1e2)

PROVISIONAL DIAGNOSIS -
Acute pancreatitis
With alcohol dependence
TREATMENT GIVEN -
1 . ivf ns and rl and dns @ 50 ml /hr
2. ink . pantop 40 mg iv/od
3 .ink zofer 4 mg iv sos
4. inj tramadol 1 amp in 100 ml na iv bd
5.inj buscopan 22 cc iv/sos
6.tab pcm 650 mg po/tid
7.grbs 6 th hourly
8 temp and i/o charting
Questions
What is the cause of shortness of breath?
What is the cause for Positive occult blood stool ?
.jpg?alt=media&token=83df6d08-0014-4540-8241-b3442c25ae3e)
.jpg?alt=media&token=0660b854-5ab5-4da7-87a4-7b421bb8a906)
.jpg?alt=media&token=75e59c89-9a75-4f8e-af9b-24060081ec4a)
.jpg?alt=media&token=0bdda955-0ecb-48fe-b02a-11ec00cdd809)
.jpg?alt=media&token=3f9fa02a-d308-492f-8b29-c8f18e81c808)
.jpg?alt=media&token=55f90537-b75e-437b-a958-c2ec48b04dd8)
.jpg?alt=media&token=0a12ba53-79d0-4886-aaaf-c71e402ad337)
.jpg?alt=media&token=b6327a61-d12c-45d4-b2c9-8f3f7c71e444)
.jpg?alt=media&token=b5549f17-041c-4db4-ba2c-bc56619bae65)
.jpg?alt=media&token=c5aacfb3-03de-42ad-9293-ab1cf88eb19c)
.jpg?alt=media&token=bf1e8b5d-db64-4cb2-9dc8-3441c6e13bb8)
.jpg?alt=media&token=8f64ba7a-6278-42d0-b8d6-f73e8bdca3f0)
.jpg?alt=media&token=27915550-305f-411a-9ccd-0484053b992e)
.jpg?alt=media&token=0bdf16f2-0495-43ff-977c-2237b9835789)
.jpg?alt=media&token=d24c3a04-a078-4ade-aef0-8c7fe7360a54)
.jpg)
.jpg?alt=media&token=ddea083a-2222-447a-b9fc-5ae4bf14aeea)
.jpg?alt=media&token=7501acb4-e96d-4bae-b888-d282701742f0)
.jpg?alt=media&token=26fe3814-335d-44d8-82c6-d87b804e039d)
_1.jpg?alt=media&token=5681bd76-2f2a-45df-a0d2-9b56000ef4e6)
.jpg?alt=media&token=56f6f250-7bd1-4ba6-8ab2-ddcb886e7ac0)
.jpg?alt=media&token=ec780e46-09c6-4cd4-be14-a6d83021e4d9)
.jpg?alt=media&token=21a229a6-b5c5-4647-b9cb-1d3b65cfc30b)
.jpg?alt=media&token=229e4783-124e-4ef0-b490-fd86e8b85d52)
.jpg?alt=media&token=9b755a9e-05fb-4220-81a8-5d55200cfb78)
.jpg?alt=media&token=d2e95639-c879-4308-a639-dff63392c694)
.jpg?alt=media&token=103fcea9-cfa6-4450-bd1c-896d1eb03aa7)
.jpg?alt=media&token=aa38e4e9-b905-4ef2-b85d-5498f9c7e25b)
.jpg?alt=media&token=fff860e3-5974-4a0e-9cc6-63bc11dd8b5d)
.jpg?alt=media&token=12c56ee3-6b38-408a-bd2a-21091bb90c61)
.jpg?alt=media&token=4046dbb6-4ef5-456c-95d1-f4ab7b64ac9e)
.jpg?alt=media&token=765b3eae-f2d9-4982-90c7-f30456eb6306)
.jpg?alt=media&token=84e6f7fb-4925-4ab9-9592-a77e54967881)
.jpg?alt=media&token=584f9e52-3ab6-4458-8e64-e63abfc2f8ca)
.jpg?alt=media&token=8011fe15-0313-4413-8bcc-c9790beb972d)
.jpg?alt=media&token=ad24f76c-35ca-48b7-a20d-c9dd1de01ff7)
.jpg?alt=media&token=3f05e5e5-bf8a-401c-a942-377fd1d62b3a)
.jpg?alt=media&token=99cd8572-1995-4095-9d27-c8ac8f7052b9)
.jpg?alt=media&token=9607b48c-be44-4985-be23-08b2dc8e8640)
.jpg?alt=media&token=a24ff8ca-67fb-4adc-a9c9-ed534340897b)
.jpg?alt=media&token=b4857393-d31c-4f5d-9684-2aedb1efdf35)

.jpg?alt=media&token=59bf3bda-2857-4ba2-89cc-dd6e9fccaf2f)
~2.jpg?alt=media&token=ed2330a4-9844-48c0-83a2-fe7a05b58566)
~2.jpg?alt=media&token=302c4101-c161-4419-8d2a-201a32e25769)

~2.jpg?alt=media&token=4f2b676c-e0b3-4bab-ace0-50c542a06534)
~2.jpg?alt=media&token=792db17a-82ba-4783-80bf-d60b26a7e1e2)
