August 27, 2021
A Shishira Reddy
4th year MBBS
21 YEAR OLD WITH FEVER AND GENERALIZED WEAKNESS.
This is an online e logbook to discuss our patients deidentified health data shared after taking her/guardian's signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs
This E log also reflects my patient centre’s online learning portfolio and valuable inputs on the comment box is welcome.
I would like to thank DR.AASHITHA for providing me with the case details.
Case:-
21 year old woman, working as a nurse in an outside hospital, presented to casualty on 26/8/2021 with the
chief complaints of
Fever since 4 months
Generalized weakness since 4 months
Body pains along with multiple joint pains since 4 months
Cough since 1 month
Vomiting 1 day back
Unable to walk since 1 day
Unable to pass urine and stool since 1 day
History of presenting illnessShe was apparently alright until 1 year back when she noticed swelling in her neck after she went for a checkup to a local hospital where she got diagnosed to be hypothyroid. She was started on Tab thyronorm 100mcg once daily.
Few months later she developed generalized weakness for which she paid a visit to a local hospital where in she was diagnosed with anemia for which she used vitamins supplementation for 2 days and stopped.
4 months back she developed low grade fever for 1 week which was nocturnal in variation, not followed by night sweats and was relieved by medications. Since then she has been experiencing
low grade fever intermittently. She started experiencing
generalized weakness and
loss of appetite.
She also tells us that she started experiencing extreme body pains to an extent that she stopped going to work. She even developed lower back pain followed by pain in her bilateral knee joints, wrists and elbow joints.
Since 1 month she has been having
cough with scanty, non blood tinged mucoid expectoration.She paid a visit to a local hospital and received symptomatic treatment for a week.
1 day back she had 2 episodes of non projectile, non bilious,
non blood tinged Vomiting.
On 26th of this month, she suddenly fell off from her bed at 7am in the morning when she tried to get up from her bed. Her mother and father had to lift her up and put her on the bed. She was unable to raise her bilateral lower limbs. Though she was able to move her toes with difficulty. Few hours later she started experiencing tingling sensation in her bilateral lower limbs. They assumed it was due to her generalized weakness and loss of appetite so she wasn't taken to any hospital. She even didn't pass urine and stool since morning. By evening after noticing that their daughter couldn't get up from her bed her parents got alarmed and got to our hospital.
On further questioning:
She gave no complains of difficulty in combing her hair, no difficulty in mixing of food.
She had difficulty in getting up or turning in the bed
She gave no complaints of loss of smell, vision, diploma or eye movements, no difficulty in chewing, loss of sensation over the face, loss of taste, hearing and swallowing.
She says that she lost around 10kgs over the past 6 months
General examination:
On presentation to us:
Thin built woman
She had pallor
Her vitals were stable
GCS - 15/15
She was conscious, coherent and cooperative with an
MMSE of 30/30
Pupils bilaterally reacting to light
Bulk - Right Left
Mid arm 18cm 18cm
Forearm 13cm 13cm
Mid thigh 26cm 26cm
Leg 18.5cm 18.5cm
Tone
UL Reduced bilaterally
LL Reduced bilaterally
Power
UL 4+/5 4+/5
LL 2/5 2/5
Reflexes
B 3+ 3+
T 2+ 2+
S 3+ 3+
K - -
A - -
P Extensor bilaterally
Abdominal reflex - Absent
Sensory system:
Priopioception lost upto the level of ankles
Vibration: Reduced in the lower limbs, more on the right side
Right Left
Great toe 3 secs 4 secs
Ankle 3 secs 8secs
Knee 6 secs 8secs
Wrist 10 secs 11 secs
Elbow 11 secs 12 secs
Fine touch - + +
Crude touch:
On right side she complained of reduced touch on her right thigh
Spinal Tenderness- present throughout all the levels of spine
Cranial nerves - normal
Cerebellar signs - absent
Lungs - Reduced breath sounds bilaterally in all the lung fields
Cvs - S1,S2 +
Per Abdomen-
Bowel sounds +
28/7/21
Her sister and mother complained of her having left eyelid ptosis and she was complaining of diplopia in the morning
Her weakness aggravated since yesterday
She also complains of neck stiffness
Neck stiffness+
Kernigs sign - couldn't be elicited as she is complaining of severe bilateral knee joint pains
Power is now 0/5 in both the lower limbs
Reflexes - Bilateral finger flexion + on Biceps and supinator examination
Lower limb reflexes absent
Abdominal reflex absent
Sensory system:
Vibration Reduced upto the level of hip joint ( lesser on the right side)
Proprioception absent upto the level of ankles
Couldn't appreciate fine and crude touch below the level of umbilicus
Left eye ptosis +
Extraocular muscles - normal
Pupils bilaterally reacting to light
All the other cranial nerves normal
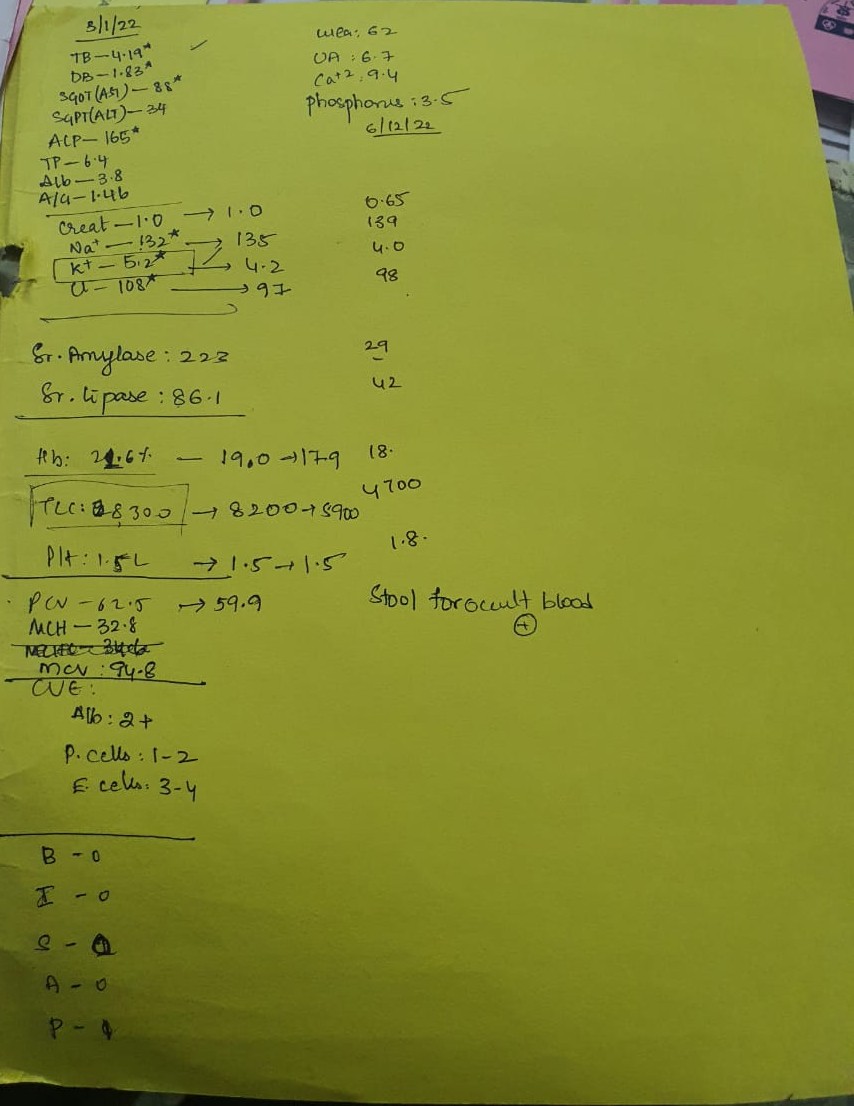
Investigations:
Hemogram:
RBC: 4.09
WBC: 12300
Hb- 8.4
PLT- 4.8 lakh
Aptt- 32 sec
PT - 16 sec
INR. - 1.11
BT - 2 min
CT - 4 min
ESR - 90 mm in 1st hr
CUE:
Albumin- nil
Sugars- nil
Pus cells - 2 to 3
Epithelial cells - 2 to 3
Blood urea- 22 mg/dl
Serum creatinine - 0.6 mg/dl
TB- 0.70 mg/dl
DB. - 0.19 mg/dl
Na+ - 132 meq/lit
K+ - 3.4 meq/lit
Cl- : 94 meq/lit
ALP: 236 IU/lit
SGOT: 13 IU/LIT
SGPT: 10 IU/LIT
Serum protein: 6.5 gm/dl
Serum magnesium: 2.2 mg/dl
Serum calcium: 9.6 mg/dl
Serum albumin: 2.4 gm/dl
Covid-19- Negative
Peripheral smear- Microcytic hypochromic anemia with leucocytosis
MRI BRAIN IMPRESSION- Acute infarct involving the genu of the corpus callosum on the left side
Provisional diagnosis:
PULMONARY KOCH'S
B/L PARAPLEGIA
HYPOPROLIFERATIVE ANEMIA SECONDARY TO NUTRITIONAL ANEMIA




 Treatment
Treatment -
On 26-08-2021:-
1) IV FLUIDS NS
2) Inj.Optineuron 1 ampoule in 100 ml NS IV/OD
3) Inj.Pan 40 mg IV/OD
On 27-08-2021:-
1) IV FLUIDS NS,RL@100ml/hr
2) Inj.Optineuron 1ampoule in 100ml NS IV OD
3) Inj.Zofer 4mg IV/TID
4) Tab.pcm 650 mg PO SOS
5) Inj.Neomol IV SOS if temp>101°f
6) Nebulization with Duolin and budecort 6th hrly
7) Syr.Ambroxol 5ml PO TID
8) TAB.Thynonorm 50 mcg PO OD
9) TAB.Ultracet PO QID
10) TAB.Ecosporin 75mg PO H/S
11) TAB.Atorvas 10 mg PO H/S
12) TAB.Clopidogrel 75 mg PO H/S
On 28-07-2021:-
1) IV FLUIDS NS,RL@100ml/hr
2) Inj.Optineuron 1ampoule in 100ml NS IV OD
3) Inj.Zofer 4mg IV/TID
4) Tab.pcm 650 mg PO SOS
5) Inj.Neomol IV SOS if temp>101°f
6) Nebulization with Duolin and budecort 6th hrly
7) Syr.Ambroxol 5ml PO TID
8) TAB.Thynonorm 50 mcg PO OD
9) TAB.Ultracet PO QID
10) TAB.Ecosporin 75mg PO H/S
11) TAB.Atorvas 10 mg PO H/S
12) TAB.Clopidogrel 75 mg PO H/S
13) Protein powder 2 spoons in 100ml milk PO /BD
On 29-08-2021:-
1) IV fluids
2) Inj optineuron 1ampoule in 100 ml NS/IV/OD
3) Inj.zofer 4mg IV/ TID
4) Inj.neomol 1g IV SOS
5) Inj methyl Prednisolone 500mg IV/OD in 100ml NS (DAY 3)
6) ATT(H-150mg R-300mg E-450mg Z-750mg)
7) Nebulization with duolin and budecort 6th hrly
8) Tab.thyonorm 50 mcg PO OD
9) Syp creamffine plus PO/TID
10) Syp ambroxal 5ml PO/TID
11) Tab ecospirin 75mg PO/OD
12) Tab atorvas 10mg PO/H/S
13) Tab Benadon 40mg PO OD
On 30-08-2021:-
1) IV fluids
2) Inj optineuron 1ampoule in 100 ml NS/IV/OD
3) Inj.zofer 4mg IV/ TID
4) Inj.neomol 1g IV SOS
5) Inj methyl Prednisolone 500mg IV/OD in 100ml NS (DAY 3)
6) ATT(H-150mg R-300mg E-450mg Z-750mg)
7) Nebulization with duolin and budecort 6th hrly
8) Tab.thyonorm 50 mcg PO OD
9) Syp creamffine plus PO/TID
10) Syp ambroxal 5ml PO/TID
11) Tab ecospirin 75mg PO/OD
12) Tab atorvas 10mg PO/H/S
13) Tab Benadon 40mg PO OD
14) Tab.Pregabiline 75mg PO H/S
On 31-08-2021:-
1) IV fluids
2) Inj optineuron 1ampoule in 100 ml NS/IV/OD
3) Inj.zofer 4mg IV/ TID
4) Inj.neomol 1g IV SOS
5) Inj methyl Prednisolone 500mg IV/OD in 100ml NS (DAY 5)
6) ATT(H-150mg R-300mg E-450mg Z-750mg)
7) Nebulization with duolin and budecort 6th hrly
8) Tab.thyonorm 50 mcg PO OD
9) Syp creamffine plus PO/TID
10) Syp ambroxal 5ml PO/TID
11) Tab ecospirin 75mg PO/OD
12) Tab atorvas 10mg PO/H/S
13) Tab Benadon 40mg PO OD
14) Tab.Pregabiline75 mgPO H/S
On 01-09-2021:
1) IV fluids
2) Inj optineuron 1ampoule in 100 ml NS/IV/OD
3) Inj.zofer 4mg IV/ TID
4) Inj.neomol 1g IV SOS
5) Tab.wysalone PO/OD
6) ATT(H-150mg R-300mg E-450mg Z-750mg)
7) Nebulization with duolin and budecort 6th hrly
8) Tab.thyonorm 50 mcg PO OD
9) Syp creamffine plus PO/TID
10) Tab ecospirin 75mg PO/OD
11) Tab atorvas 10mg PO/H/S
12) Tab Benadon 40mg PO OD
13) Tab.Pregabiline 75mg PO H/S
14) Tab.levipil 250 mg PO/BD
On 02-09-2021:-
1) IV fluids
2) Inj optineuron 1ampoule in 100 ml NS/IV/OD
3) Inj.zofer 4mg IV/ TID
4) Inj.neomol 1g IV SOS
5) Tab.wysalone PO/OD
6) ATT(H-150mg R-300mg E-450mg Z-750mg)
7) Nebulization with duolin and budecort 6th hrly
8) Tab.thyonorm 50 mcg PO OD
9) Syp creamffine plus PO/TID
10) Tab ecospirin 75mg PO/OD
11) Tab atorvas 10mg PO/H/S
12) Tab Benadon 40mg PO OD
13) Tab.Pregabiline 75mg PO H/S
14) Tab.levipil 250 mg PO/BD
Questions
1) Is pulmonary koch's a cause for nutritional anemia and generalized weakness?
2) what is the possible cause of infarction in the left side corpus callosum?
3) what is the cause of paraplegia in the patient?
.jpg?alt=media&token=83df6d08-0014-4540-8241-b3442c25ae3e)
.jpg?alt=media&token=0660b854-5ab5-4da7-87a4-7b421bb8a906)
.jpg?alt=media&token=75e59c89-9a75-4f8e-af9b-24060081ec4a)
.jpg?alt=media&token=0bdda955-0ecb-48fe-b02a-11ec00cdd809)
.jpg?alt=media&token=3f9fa02a-d308-492f-8b29-c8f18e81c808)
.jpg?alt=media&token=55f90537-b75e-437b-a958-c2ec48b04dd8)
.jpg?alt=media&token=0a12ba53-79d0-4886-aaaf-c71e402ad337)
.jpg?alt=media&token=b6327a61-d12c-45d4-b2c9-8f3f7c71e444)
.jpg?alt=media&token=b5549f17-041c-4db4-ba2c-bc56619bae65)
.jpg?alt=media&token=c5aacfb3-03de-42ad-9293-ab1cf88eb19c)
.jpg?alt=media&token=bf1e8b5d-db64-4cb2-9dc8-3441c6e13bb8)
.jpg?alt=media&token=8f64ba7a-6278-42d0-b8d6-f73e8bdca3f0)
.jpg?alt=media&token=27915550-305f-411a-9ccd-0484053b992e)
.jpg?alt=media&token=0bdf16f2-0495-43ff-977c-2237b9835789)
.jpg?alt=media&token=d24c3a04-a078-4ade-aef0-8c7fe7360a54)
.jpg)
.jpg?alt=media&token=ddea083a-2222-447a-b9fc-5ae4bf14aeea)
.jpg?alt=media&token=7501acb4-e96d-4bae-b888-d282701742f0)
.jpg?alt=media&token=26fe3814-335d-44d8-82c6-d87b804e039d)
_1.jpg?alt=media&token=5681bd76-2f2a-45df-a0d2-9b56000ef4e6)
.jpg?alt=media&token=56f6f250-7bd1-4ba6-8ab2-ddcb886e7ac0)
.jpg?alt=media&token=ec780e46-09c6-4cd4-be14-a6d83021e4d9)
.jpg?alt=media&token=21a229a6-b5c5-4647-b9cb-1d3b65cfc30b)
.jpg?alt=media&token=229e4783-124e-4ef0-b490-fd86e8b85d52)
.jpg?alt=media&token=9b755a9e-05fb-4220-81a8-5d55200cfb78)
.jpg?alt=media&token=d2e95639-c879-4308-a639-dff63392c694)
.jpg?alt=media&token=103fcea9-cfa6-4450-bd1c-896d1eb03aa7)
.jpg?alt=media&token=aa38e4e9-b905-4ef2-b85d-5498f9c7e25b)
.jpg?alt=media&token=fff860e3-5974-4a0e-9cc6-63bc11dd8b5d)
.jpg?alt=media&token=12c56ee3-6b38-408a-bd2a-21091bb90c61)
.jpg?alt=media&token=4046dbb6-4ef5-456c-95d1-f4ab7b64ac9e)
.jpg?alt=media&token=765b3eae-f2d9-4982-90c7-f30456eb6306)
.jpg?alt=media&token=84e6f7fb-4925-4ab9-9592-a77e54967881)
.jpg?alt=media&token=584f9e52-3ab6-4458-8e64-e63abfc2f8ca)
.jpg?alt=media&token=8011fe15-0313-4413-8bcc-c9790beb972d)
.jpg?alt=media&token=ad24f76c-35ca-48b7-a20d-c9dd1de01ff7)
.jpg?alt=media&token=3f05e5e5-bf8a-401c-a942-377fd1d62b3a)
.jpg?alt=media&token=99cd8572-1995-4095-9d27-c8ac8f7052b9)
.jpg?alt=media&token=9607b48c-be44-4985-be23-08b2dc8e8640)
.jpg?alt=media&token=a24ff8ca-67fb-4adc-a9c9-ed534340897b)
.jpg?alt=media&token=b4857393-d31c-4f5d-9684-2aedb1efdf35)

.jpg?alt=media&token=59bf3bda-2857-4ba2-89cc-dd6e9fccaf2f)
~2.jpg?alt=media&token=ed2330a4-9844-48c0-83a2-fe7a05b58566)
~2.jpg?alt=media&token=302c4101-c161-4419-8d2a-201a32e25769)

~2.jpg?alt=media&token=4f2b676c-e0b3-4bab-ace0-50c542a06534)
~2.jpg?alt=media&token=792db17a-82ba-4783-80bf-d60b26a7e1e2)





